Temporal trends in sperm count: a systematic review and meta-regression analysis of samples collected globally in the 20th and 21st centuries
Abstract
Numerous studies have reported declines in semen quality and other markers of male reproductive health. Our previous meta-analysis reported a significant decrease in sperm concentration (SC) and total sperm count (TSC) among men from North America–Europe–Australia (NEA) based on studies published during 1981–2013. At that time, there were too few studies with data from South/Central America–Asia–Africa (SAA) to reliably estimate trends among men from these continents.
The aim of this study was to examine trends in sperm count among men from all continents. The broader implications of a global decline in sperm count, the knowledge gaps left unfilled by our prior analysis and the controversies surrounding this issue warranted an up-to-date meta-analysis.
We searched PubMed/MEDLINE and EMBASE to identify studies of human SC and TSC published during 2014–2019. After review of 2936 abstracts and 868 full articles, 44 estimates of SC and TSC from 38 studies met the protocol criteria. Data were extracted on semen parameters (SC, TSC, semen volume), collection year and covariates. Combining these new data with data from our previous meta-analysis, the current meta-analysis includes results from 223 studies, yielding 288 estimates based on semen samples collected 1973–2018. Slopes of SC and TSC were estimated as functions of sample collection year using simple linear regression as well as weighted meta-regression. The latter models were adjusted for predetermined covariates and examined for modification by fertility status (unselected by fertility versus fertile), and by two groups of continents: NEA and SAA. These analyses were repeated for data collected post-2000. Multiple sensitivity analyses were conducted to examine assumptions, including linearity.
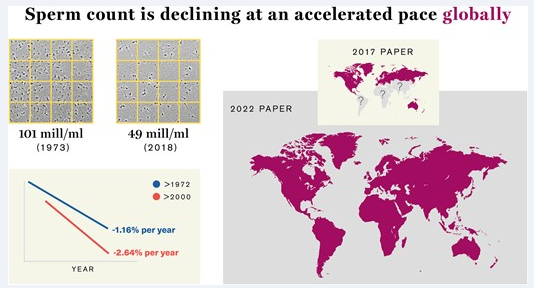
Overall, SC declined appreciably between 1973 and 2018 (slope in the simple linear model: –0.87 million/ml/year, 95% CI: –0.89 to –0.86; P < 0.001). In an adjusted meta-regression model, which included two interaction terms [time × fertility group (P = 0.012) and time × continents (P = 0.058)], declines were seen among unselected men from NEA (–1.27; –1.78 to –0.77; P < 0.001) and unselected men from SAA (–0.65; –1.29 to –0.01; P = 0.045) and fertile men from NEA (–0.50; –1.00 to –0.01; P = 0.046). Among unselected men from all continents, the mean SC declined by 51.6% between 1973 and 2018 (–1.17: –1.66 to –0.68; P < 0.001). The slope for SC among unselected men was steeper in a model restricted to post-2000 data (–1.73: –3.23 to –0.24; P = 0.024) and the percent decline per year doubled, increasing from 1.16% post-1972 to 2.64% post-2000. Results were similar for TSC, with a 62.3% overall decline among unselected men (–4.70 million/year; –6.56 to –2.83; P < 0.001) in the adjusted meta-regression model. All results changed only minimally in multiple sensitivity analyses.
This analysis is the first to report a decline in sperm count among unselected men from South/Central America–Asia–Africa, in contrast to our previous meta-analysis that was underpowered to examine those continents. Furthermore, data suggest that this world-wide decline is continuing in the 21st century at an accelerated pace. Research on the causes of this continuing decline and actions to prevent further disruption of male reproductive health are urgently needed.

Sperm count is declining at an accelerated pace globally.
Introduction
In 2017, ‘Temporal Trends in Sperm Count: A Systematic Review and Meta-Regression Analysis’ was published by this journal (Levine et al., 2017). That article, which was widely discussed and highly cited, includes all eligible English-language publications in 1981–2013 that contained data on sperm count. We reported a very strong decline in sperm concentration (SC) and total sperm count (TSC) in North America, Europe, Australia/New Zealand (hereafter NEA) but too few studies have been published in South/Central America, Asia and Africa (hereafter SAA) to draw a conclusion about trends in those continents. We examined mean SC and TSC as a function of collection year, as approximated by the mid-year of the sample collection period. Because sample collection preceded the year of publication by an average of 6 years, our results were already somewhat dated by the time we published our analysis in 2017. Therefore, we conducted a new literature search in the spring of 2020 to identify eligible studies published between 1 January 2014 and 31 December 2019. Here, we report on global trends in SC and TSC in publications 1981 through 2019, which combines results of both searches and analyses. This expanded analysis addresses two important questions. With increased sample size, was a trend seen in South America, Africa and Asia? Did the trends we reported continue post-2011?
Recognition of the importance of male reproductive function, and sperm count, has increased since 2017 (Levine et al., 2018; United Nations Human Rights Office of the High Commissioner, 2019). The economic and societal burden of male infertility is now widely recognized, as is the unequal burden of male infertility which falls most heavily on low-income populations (Winters and Walsh, 2014; Hauser et al., 2015; Dupree, 2016; Skakkebaek et al., 2016). Increasingly strong evidence links reduced sperm count and concentration to increases in all-cause mortality and morbidity (Latif et al., 2017; Del Giudice et al., 2021; Ferlin et al., 2021). Links between sperm count and infertility are well-recognized (Bonde et al., 1998; Skakkebæk et al., 2022). Furthermore, the decline in sperm count is paralleled by declines in testosterone and increases in testicular cancer and male genital anomalies (Skakkebæk et al., 2022). In fact, the decline in semen quality and male reproductive health has recently been described as a crisis (De Jonge and Barratt, 2019). Relative to declines in sperm counts, these latter trends are far more difficult to document. There is currently no systematic collection of such data, making the examination of those trends difficult. Therefore, an international group of scientists, including several of the authors, has suggested the formation of a multidisciplinary monitoring system for reproductive health indicators that would provide ongoing surveillance of reproductive health outcomes (Le Moal et al., 2016).
The broad implications of a global decline in sperm count, the data gaps left unfilled by our prior analysis and the controversies surrounding these issues warrant an up-to-date meta-analysis. This meta-analysis was conducted to address these aims.
Methods
This systematic review and meta-regression analysis was conducted, and the results reported, in accordance with Meta-analysis in Observational Studies in Epidemiology (Stroup et al., 2000) (Supplementary Table SI) and Preferred Reporting Items for Systematic reviews and Meta-Analysis guidelines (Liberati et al., 2009; Moher et al., 2009). Our research team included epidemiologists, andrologists and a medical librarian. Our predefined protocol was developed following best practices (Borenstein et al., 2009; Higgins and Green 2011; National Toxicology Program 2015) and informed by our previous study. Throughout, unless otherwise noted, the methods of the current study are those employed and published in the previous study (Levine et al., 2017), including keywords and databases searched, eligibility criteria and statistical methods.
Systematic review and study selection
A comprehensive search of the PubMed/MEDLINE and EMBASE was conducted, to identify English-language publications that reported primary data on human sperm count, published in 2014–2019, i.e. from the last date included in our prior search through 2019. On 15 May 2020, we searched MEDLINE/PubMed and Embase (Excerpta Medica database) for peer-reviewed publications meeting our inclusion criteria. Following the recommendation of the Cochrane Handbook for Systematic Reviews, we searched in title and abstract for both index (MeSH) terms and keywords and filtered out animal-only studies. We used the MeSH term ‘sperm count’, which includes seven additional terms, and to increase sensitivity, we added 13 related keywords (e.g. ‘sperm density’, ‘sperm concentration’).
All English-language studies that reported primary data on human SC were considered eligible for abstract screening. We evaluated the eligibility of all subgroups within a study. For example, in a case–control study, the control group might have been eligible for inclusion even though, based on our exclusion criteria, the case group was not.
We divided eligible studies into two fertility-defined groups: (i) studies of men unselected by fertility status, hereafter ‘Unselected’ (e.g. young men unlikely to be aware of their fertility, such as young men being screened for military service or college students) and (ii) studies of men whose partners had born a child or whose partners were pregnant regardless of pregnancy outcome, hereafter ‘Fertile’. ‘Total’ refers to both groups.
A study was excluded if participants were selected based on: (i) infertility or sub-fertility; (ii) their range of semen parameters (e.g. studies selecting normospermic men); and (iii) genital abnormalities, diseases or medications. We also excluded studies limited to men with exposures that may affect fertility, such as an occupational exposure, post-clinical trial intervention or smoking. Studies of candidates for vasectomy or semen donation were included only if semen quality was not a criterion for men’s study participation. We excluded studies that used non-standard methods for sperm collection (e.g. methods other than masturbation) or counting methods other than hemocytometer and studies with fewer than 10 men.
First, the publication was either excluded or advanced to full-text screening based on the title and abstract. Any publication without an abstract was automatically referred for full-text screening. Second, we reviewed the full text and assigned it to exclusion (and categorized the reason for exclusion) or to data extraction. We then confirmed study eligibility and identified multiple publications from the same study to ensure that estimates from the same population were not used more than once.
Data extraction
For each estimate, we extracted summary statistics on SC and TSC (mean, standard deviation, minimum, maximum, median and percentiles), semen volume (mean and measured method), sample size, sample collection years, data on covariates (fertility group, country, age, ejaculation abstinence time reported and per protocol, method of semen collection, method of assessing of SC and semen volume, selection of population, study exclusion criteria and number of samples per man). The range of permissible values, both for categorical and numerical variables and information on data completeness were recorded. Data were extracted on the total population as well as on all eligible subgroups.
Quality control
The current study followed the same protocol as used in the previous study. For the new search, we used Covidence systematic review software for the process of screening the articles that were not available for our prior search. In addition, one member of the research team was replaced. Screening of this extensive systematic review was conducted by a team of eight reviewers (H.L., N.J., A.M.-A., J.M., D.W.-D., M.J., R.P., S.H.S.). As in our previous analysis, the screening protocol was piloted and reviewers were trained by screening of 50 abstracts by all reviewers followed by a comparison of results, resolution of any inconsistencies and clarification of the protocol as needed. The same quality control process was followed for full-text screening and data extraction by all reviewers. All data were entered into digital spreadsheets with explicit permissible values (no open-ended entries) to increase consistency. After data extraction, an additional round of data editing and quality control of all studies was conducted by H.L. and M.J. The process ensured that each study was evaluated by at least two different trained reviewers.
Source Link: https://academic.oup.com/humupd/advance-article/doi/10.1093/humupd/dmac035/6824414
Bitchute: https://www.bitchute.com/channel/YBM3rvf5ydDM/
Telegram: https://t.me/Hopegirl587
EMF Protection Products: www.ftwproject.com
QEG Clean Energy Academy: www.cleanenergyacademy.com
Forbidden Tech Book: www.forbiddentech.website